Cervical Screening / Vulval Pathology Flashcards
identify the cells present within normal ectocervix?

what does the endocervix normally look like histologically?

what is the transformation zone and which physiological changes causes the altering of position of TZ during life?
squamo-columnar junction between ectocervical (squamous) and endocervical (columnar) epithelia
position of TZ alters in response to menarche, pregnancy and menopause
what does the squamo-columnar junction look like histologically?
what is cervical erosion?
the exposure of delicate endocervical epithelium to acid environment of vagina leads to physiological squamous metaplasia
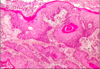
what are nabothian follicles?
mucous filled cyst on surface of cervix - formed when stratified squamous epithelium of ectocervix (nearest vagina) grows over columnar epithelium of endocervix (portion nearest to uterus)
what are the symptoms and causes of cervicitis?
often asymptomatic but can lead to infertility due to simultaneous sildent fallopian tube damage
causes - non specific inflammation, follicular cervicitis (sub epithelial reactive lymphoid follicles present in cervix), chlamydia and HSV
what is a cervical polyp and what is the main symptom?
localised inflammatory outgrowth (not premalignant)
cause of bleeding, if ulcerated
what are the different neoplastic causes of cervical pathology?
cervical intraepithelial neoplasia (CIN)
cervical cancer = squamous carcinoma, adenocarcinoma
what are the risk factors for CIN / cervical cancer?
high risk HPV esp 16 and 18 (sexual partners may increase risk)
vulnerability of SC junction in early reproductive lise - age at first intercourse, long term use of OCP, non use of barrier contraception
smoking - 3x risk
immunosuppression
what strains of HPV causes genital warts and what does this look like histologically?
HPV 6 and 11
condyloma acuminatum = thickened “papillomatous” squamous epithelium with cytoplasmic vacuolation (koliocytosis)
what strains of HPV causes cervical intraepithelial neoplasia (CIN) and what does this look like histologically?
HPV 16 and 18
infected epithelium remains flat, but may show koilocytosis, which can be detected in cervical smears

what does cervical cancer look like histologically?
invasive squamous carcinoma - virus integrated into host DNA
how long does it take for HPV infection to progress to high grade CIN?
6 months - 3 years
how long does it take for high grade CIN to become invasive cancer?
5-20 years
what does mild dyskaryosis with viral features (HPV) look like?

what is cervical intraepithelial neoplasia (CIN) and where does it occur?
pre-invasive stage of cervical cancer - dysplasia of squamous cells which is not visible by naked eye and is asymptomatic
occurs at transformation zone
detected by cervical screening
describe the progressive degrees of dysplasia and neoplasia of cervix?
normal squamous epithelium -> koilocytosis -> CIN1 -> CIN2 -> CIN3