Hemodynamics 1 and 2 Flashcards
1
Q
Role of the Cardiovascular System (9)
A
- Move oxygen from the lungs to all body cells
- Move nutrients and water from the gastrointestinal system to all body cells
- Move metabolic wastes from all body cells to kidney for excretion
- Move heat from cells to skin for dissipation
- Move carbon dioxide from body cells to lungs for elimination
- Move particular toxic substances from some cells to liver for processing
- Move hormones from endocrine cells to their targets
- Move stored nutrients from liver and adipose tissue to all cells
- Carries immune cells, antibodies, and clotting proteins to wherever they are needed
2
Q
Pulmonary vs. Systemic Circulation
A
- Pulmonary
- Right heart –> lungs
- Permit gas exchange (oxygenation of the blood and removal of CO2)
- Systemic
- Left heart –> body (except lungs)
- Perfuses all the cells of the body
3
Q
Anatomy of the Cardiovascular System
A
- Superior and inferior vena cava
- Blood is blue b/c carries less oxygen than blood in systemic circulation
- Right atrium
- Tricuspid valve
- Assures unidirectional blood flow
- Right ventricle
- Pulmonary semilunar valve
- Pulmonary arteries
- Lungs
- Blood is oxygenated
- Pulmonary veins
- Left atrium
- Bicuspid (mitral) valve
- Left ventricle
- Aortic semilunar valve
- Aorta
- Distributes oxygenated blood throughout body
4
Q
What heart is enclosed in and mainly comprised of
A
- Heart is enclosed in a tough membranous sac: pericardium
- Heart is mainly comprised of cardiac muscle: myocardium
5
Q
Matching of Pulmonary and Systemic Blood Flow
A
- Volume of blood leaving left and right heart per unit time must be matched
- Otherwise, fluid would accumulate in one system
- Ex. Severely damaged left ventricle (congestive heart failure)
- Blood would accumualte in pulmonary circulation
- –> impairment of gas exchange in the lungs
6
Q
Blood
A
- Liquid medium: plasma
- 50-55% blood volume
- Contains plasma proteins (albumin, globulin), electrolytes, hormones, enzymes, and blood gases
- Formed elements
-
Red cells (erythrocytes)
- 40-45% total blood volume
- Centrifuged: settle to bottom
- Hematocrit: volume of RBCs in blood
- Contain hemoglobin: bind w/ & transport oxygen
-
White cells (leukocytes)
- 5% total blood volume
- Centrifuged: settle on top of red cells
- For immune processes & bodily defense
-
Platelets
- Little blood volume
- For blood coagulation
-
Red cells (erythrocytes)
7
Q
Fluid Flow & Pressure
A
- Fluid moves form regions of higher pressure to regions of loewr pressure
- Contraction of ventricles imparts pressure
- Friction is lost as blood flows through blood vessels

8
Q
Ohm’s Law
A
- ( Q = ΔP/R ) or ( ΔP = Q * R ) or ( R = ΔP/Q )
- ΔP = change in pressure on two ends of a vessel (not within the vessel itself)
- Q = blood flow
- R = resistance
- Flow through a vessel will be directly proportional to pressure and inversely proportional to resistance
- Ex. if you increase the length of a vessel, you increase resitance and decrease flow
9
Q
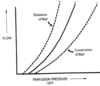
Poiseuille’s Law
A
- Q = πΔPr4/ 8ηl
R = 8ηl / πr4- Q = flow
- π/8 is a constant
- ΔP = the pressure driving force
- r = radius of the vessel
- η = viscosity of the fluid
- l = length of the vessel
- Explains the flow of fluid through tubes of different sizes
- A change in radius has a huge effect on blood flow
- If halve the radius, you decrease blood flow by 16x
- Only valid under conditoins of laminar flow
10
Q
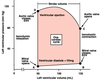
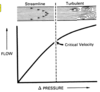
Laminar vs. Turbulence / Tubulent Flow
A
- Laminar flow
- Fluid on the inside moves faster than the fluid on the outside of a vessel
- Large vessel: fluid flows faster
- Small vessel: fluid flows slower
- Ex. normal blood flow
- Turbulence
- As flow velocity increases, eventually a criticla velocity is reached at which the concentric layers break down
- –> side-to-side motion of fluid
- Increased turbulence –> increased viscosity –> decreased flow
- Turbulent Flow
- Frictional resistance is increased
- The bigger the vessel (increased diameter) and the quicker the blood flow (increased velocity), the more likely turbulent flow will occur
- Sounds which emanate from the circulatory system (murmurs) are the result of localized turbulence
11
Q
Reynold’s Number (Re)
A
- Re = dvD/η
- d = fluid density
- v = velocity
- D = tube diameter
- η = viscosity
- Critical Re = 1000
-
Re < 1000 –> laminar flow
- Smaller vessels
- Decreased velocity
-
Re > 1000 –> turbulen flow
- Larger vessels
- Increased velocity
12
Q
Poiseuille’s Law and Vasodilation/Vasoconstriction
A
- Can affect blood flow by altering blood vessel size via vasodilation/vasoconstriction
- Vasodilation –> decreased resistance –> increased blood flow
- Vasoconstriction –> increased resistance –> decreased blood flow
13
Q
Poiseuille’s Law and Hematocrit
A
- Increased hematocrit –> increased viscosity –> increased resistance –> decreased blood flow
- Anemia: low hematocrit, increased blood flow
- Polycythemia: high hematocrit, decreased blood flow
14
Q
Blood Pressure: Systole, Diastole, Pulse, Pulse Pressure
A
- Systole: cardiac muscle contracts
-
Diastole: cardiac muscle relaxes
- Lasts 2x as long as systole
- If heart rate = 67
- Cardiac cycle = 900 ms
- Diastole = 600 ms
- Systole = 300 ms
- Pulse: wave transmitted when the left ventricle contracts
-
Pulse pressure: amplitude of pulse wave
- Depends on the volume of blood ejected and the compliance of the arteries
15
Q
Blood Pressure: Potential vs. Kinetic Energy
A
- Arteries contain fibrous and elastic connective tissue
- When high-pressure blood contacts arterial walls, potential energy is absorbed when the artery becomes stretched
- Energy is released as kinetic energy through elastic recoil
- Process limits the drop in arterial pressure during diastole
- Flow of blood from arteries to capillaries is continuous even though the flow from ventricle to aorta is pulsatile