Reisert: Dementia and Delerium Flashcards
acute confusional state with decreased attention that usually lasts over hours to days, but may last months to years
Delirium
Also known as:
- confusion
- encephalopathy
- acute brain failure
- acute confusional state
Delirium
- Older age, baseline dysfunction (failing health, dementia, nursing home patients)
- poor sleep
- hospitalization (Catheters, restraints, sleep deprivation, multiple meds, pain)
Epidemiology of Delirium
Decreased attention is KEY
May have additional sx:
- change in sleep awake cycles
- hallucinations
- delusions
- ANS changes such as HR or BP problems
- hypo or hyperactive status
PE features of Delirium
- Usually due to diffuse cerebral dysfunction
- May be r/t low Ach levels
- May mimic Alzheimer’s, Lewy body dementia
- High dopamine levels possible
Pathology of Delirium
Clinical at bedside
Compare baseline function (ask family)
Check for medications:
- anti-cholinergics
- sedatives/narcotics/benzodiazepines
Diagnosis of Delirium
- ICU/ Post-op psychosis
- Sundowning
- Delirium tremens
Delirium syndromes
Illness:
sepsis, fever, dehydration, drug abuse
Causes of ICU/Post-op psychosis
Old people who get worse at night
- common
- worse if underlying mental health issues, especially dementia
Various degrees of delirium
Sundowning
Maintain day-awake cycle
Night-sleep normalcy
Reassurance/reorientation
Treatment of sundowning
Mild:
- Tremor
- Agitation, anxiety
DT’s
- Intense reaction
Sx of alcohol withdrawal
Usually begins 5-10 hours after cessation
Peaks 2-3 days after cessation
Alcohol withdrawal
Alcohol withdrawal syndrome that is worse in context of illness (hospitalization)
Delirium tremens
- Agitation
- Tremor
- Hallucinations
- ANS instability (increased BP, pulse, resp)
- Seizures
Sx of Delirium tremens
treat as status epilepticus
Tx for seizures during Delirium tremens
Don’t drink
Slow taper off EtOH
Safe enviro/reoreintation/family, B vitamins, hydrate, treat illnesses
Benzodiasepines
Phenobarbital (less proof?)
Prevention of delirium tremens
- Benzo’s
- Longer acting better
- Diazepam (Valium)
- Chlordiazepoxide (Librium)
- IV or PO
- Bad DT’s: high dose
- Longer acting better
- Phenobarbital
- Antipsychotics
- Haloperidol (Haldol)
Tx of delirium tremens
Infection
Sepsis
Drugs
Medications
Reversible causes of delirium
HIgh mortality and morbidity
23-33% die (same incidence as sepsis)
longer length of stay
Outcomes of delirium
- Toxins
- Metabolic
- liver, kidney, electrolytes, glucose
- Infection
- Endocrine
- thyroid, Vit. B12 def.
- Cerebrovascular
- stroke, seizure/post-ictal, metastasis, HoTN
- Vasculitis
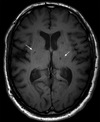
Delirium workup
Labs (basics-case specific)
Imaging RARELY helpful
Lumbar puncture
EEG to r/o seizures
Delirium workup
Case by case directed-very difficult
Supportive (reorientation, safety)
Day/night normalcy
Home like enviro
bed alarms/sitters
Antipsychotics (Haldol, new “Atypicals”)
Benzo’s (not as good-sedation)
Bedrails
Tx of delirium
>4M americans
>$100B annual cost
Dementia
“Benign forgetfulness of elderly”
May progress to mild cognitive impairment
Can later develop in some
Dementia
Memory loss
10% >70 y/o
20-40% >85 y/o
Dementia
Continuum of diease with KEY features
Memory loss (KEY)
Other problems that develop later:
Speech and language difficulties, problem solving difficulties, impaired judgement, mood issues
Often progresive
Dementia
Mood disturbances may or may not be seen
- Depression
- Agitation
- Delusions
- Insomnia
- Disinhibition
Dementia
Changes in cerebral circuits
Nerve loss
Changes in neurotransmitters: Acetylcholine, serotonin, glutamine
Neurological features of dementia
Age: by far the greatest
Viral: Creutzfeldt-Jakob
Genetics?: FH of presence of apolipoprotein ε4-a mutant apolipoprotein that may have implications in amyloid formation
Risk factors for dementia