Sepsis and Septic Shock Flashcards
What is systemic inflammatory response syndrome (SIRS)?
Widespread inflammatory response to a variety of clinical insults. This can include things like pancreatitis, burns and trauma
What clinical parameters are assessed to determine if someone has SIRS?
- Temperature
- Heart Rate
- Respiratory rate
- WBC count
When assessing temperature in the criteria for SIRS, what threshold(s) is/are used?
- >38oC
- <36oC
Whan assessing heart rate in the criteria for SIRS, what HR thershold (s) is/are used?
>90bpm
When assessing respiratory rate in the criteria for SIRS, what thershold (s) is/are used?
>20 breaths/minute
OR
PaCO2 <32
When assessing the WBC count in the criteria for SIRS, what threshold(s) is/are used?
- >12000 cells/mm3
- <4000 cells/mm3
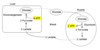
What is the definition of sepsis?
SIRS plus infection
Life-threatening organ dysfunction caused by dysregulated host repsonse to infection

What is the definition of severe sepsis?
Sepsis plus End organ damage

What is the definiton of septic shock?
Severe sepsis plus Hypotension unresponsive to fluids
Can be identified with a clinical construct of sepsis with persisting hypotension requiring vasopressors to maintain MAP >65mmHg and having a serum lactate of >2mmol/l despite adequate volume resuscitation

What occurs in phase 1 of sepsis pathophysiology?
Release of bacterial toxin
- Endotoxin - LPS
- Exotoxin - superantigen
What occurs in phase 2 of sepsis pathophysiology?
Mediator relsease in response to infection
- Pro-inflammatory cytokines - cause inflammatory response
- Anti-inflammatory sytokines - keeps pro-inflammatory response in check
What chemical is released in response to vascular endothelial damage caused by infectious organisms?
Nitric oxide - chemical vasodilator

What pathway is activated by bacterial toxins?
Complement pathway - stimulates mast cells

What chemical do mast cells release in repsonse to activation by the complement pathway?
Histamine
What are the main pro-inflammatory cytokines released by macrophages nad neutrophils in response to bacterial toxin release?
- TNF
- IL-1

What chemicals do the endothelial cells release in response to being stimulated by TNF and IL-1?
Release of reactive oxygen species and platelet activating factor

What is the overall outcome on vascular structure and permeability in response to pro-inflammatory cytokine release?
- Damage and increased permeability
- Net increase in clotting
What are the effects of pro-inflammatory mediators?
- Promote endothelial cell – leukocyte adhesion
- Release of arachidonic acid metabolites
- Complement activation
- Vasodilatation of blood vessels by NO
- Increase coagulation - release of tissue factors and membrane coagulants
- Cause hyperthermia
What are the effects of anti-inflammatory mediators?
- Inhibit TNF alpha
- Augment acute phase reaction
- Inhibit activation of coagulation system
- Provide negative feedback mechanisms to pro-inflammatory mediators
What is the difference between septic shock and immunoparalysis in terms of pro-inflammatory and anti-inflammatory cytokines?
- Septic shock - compensatory mechisms are outweighed by pro-inflammatory mechanisms
- Immunoparalysis - Compensatory mechanisms outweigh pro-inflammatory mechanisms