9. Development and Sexual Differentiation of the Reproductive System Flashcards
(18 cards)
When and how does gonadal development of male and female begin?
What are the developing male and female ducts called, and where do they empty into?
What do primordial germ cells do?
Week 5, begins as masses of mesoderm - gonadal ridges which form bulges on dorsal abdominal wall medial to mesonephros (developing temporary kidney)
Female: Mullerian ducts (paramesonephric). Male: Wolffian ducts (medonephric). Both empty into common cloaca.
Migrate to and seed developing gonads with stem cells which become spermatogonia or oogonia. Gonadal ridges will form testes or ovaries.
Label A-F (at 5-6 weeks)

A) mesonephros
B) gonadal ridges
C) metanephros (kidney)
D) Wolffian duct (mesonephric)
E) Mullerian duct (paramesonephric)
F) Cloaca
Describe how the internal reproductive organs start to develop in a 7-8 week old male.
Inguinal canals develop in both sexes because of indifferent state of sexual development. Describe how they develop.
What does the gubernaculum do in the developing male?
Seminiferous tubules form in gonadal ridge and join Wolffian duct via efferent ductules. Testes secrete anti-Mullerian hormone.
A gubernaculum descends on each side of the abdomen from inferior pole of the gonad and passes obliquely through anterior abdominal wall at the site of the future inguinal canal. It attaches caudally to the internal surface of the labioscrotal swellings (future scrotum/labia majora)
Pulls testes down through anterior abdominal wall to the scrotal swelling. (Peritoneum sticks to it as it descends)

What is the processus vaginalis, and where does it develop?
What does the processus vaginalis form in males?
How long and when does descent of the testes occur?
What is the inguinal canal?
Evagination of peritoneum, develops ventral to gubernaculum and herniates through abdominal wall along path formed by gubernaculum.
It carries extensions of layers of the anterior abdominal wall - forms the walls of the inguinal canal.
Through inguinal canal, takes 2-3 days, happens around week 26, 97% of full term boys have both descended, during 3m most others descend.
2mm above inguinal ligament, starts at deep inguinal ring (midinguinal point) and emerges at superficial inguinal ring

Where do testicular blood vessels origionate from?
What is cryptorchidism?
What are ectopic testes?
Abdominal aorta or renal vessels. Blood supply to gonads from L2-L3. Male around pelvic rim to deep inguinal ring; female ovarian vessels have different distal course.
Absence of one or both testes from the scrotum, in 3-4% full term and up to 30% premature. If testes remain in abdomen = sterility. Normally in inguinal canal and often descend spontaneously. Can have surgery to make it descend.
Rare, interstitial ectopia occurs most frequently, when gubernaculum passes to abnormal location
What is a congenital (indirect) hernia?
What is a hydrocele?
What is the vas deferens?
If communication between tunica vaginalis and peritoneal cavity fails to close, persistant processus vaginalis exists. A loop of intestine herniates through deep inguinal ring and passes through the inguinal canal.
Processus vaginalis remains open but is too small to allow herniation, but there is accumulation of peritoneal fluid either in the spermatic cord or testes.
Transport sperm from the epididymis to the ejaculatory ducts. Spermatic cord -> inguinal canal -> runs on lateral pelvic wall covered by perineum, crosses external iliac vessels and ureter, at ischial spine descends behind bladder.

What are seminal vesicles?
Is a patient completely sterile after a vasectomy?
Coiled, sacculated diverticulum of vas deferens. Creates and secretes spermatic fluid. Seperated from rectum behind by rectovesical fascia and rectovesical pouch.
No, not for 3-6m after because of sperm in vesicles. (Deferens cut and tied/sealed)
Label A-G

A) prostate
B) pubic symphysis
C) external urinary sphincter
D) rectovesical pouch
E) seminal vesicle
F) common ejaculatory duct
G) Cowper’s gland
Breifly describe the prostate.
What is prostatic hypertrophy?
Prostatic cancer commonly affects which lobe?
Below bladder on pelvic floor, 1 median and 2 lateral lobes, traversed by urethra and ejaculatory duct.
Prostate enlarges esp. median lobe - disturbs vesicular sphincter action and renders micturition difficult. TURP (transurethral resection of prostate) permits coring out of median lobe.
Lateral lobes, may be felt as hard irregular mass on rectal examination.
Describe how the internal reproductive organs start to develop in a 7-8 week old female.
What is the ovarian ligament (cranial gubernaculum) and the round ligament (caudal gubernaculum)?
What are some abnormalities of the female genital tract (Mullarian duct anomilies)?
Mullarian (paramesonephric) ducts differentiate into ducts of female duct system, and Wolffian ducts (mesonephric) degenerate. Ovaries descend on the gubernaculum from posterior abdominal wall to pelvic brim, where their progress is stopped by the broad ligament.
Ovarian ligament: ovary -> uterus. Round ligament: uterus -> labia majora via inguinal canal.
Double uterus/bicornuate/unicornuate uterus results from incomplete fusion of Mullerian ducts inferiorly, incomplete development of the ducts, or failure of one of the ducts.

What is the vestigal gubernaculum? How does it support the uterus?
Where does the ovarian blood supply origionate from? Where are they found?
Where do the veins drain back to on the L and R?
The round ligament of the uterus. Helps keep uterus anteverted (leaning) and anteflexed (bent over bladder).
Abdominal aorta or renal vessels. Retroperitoneally over pelvic brim superficial to iliac vessels. In suspensory ligament of ovary (in females).
R: drain to inferior vena cava. L: drain to L renal vein. Like in men, who can have varicocele (varicose veins in testes) - most common on L b/c venous drainage to L - higher pressure
Label A-C

A) ovarian ligament
B) round ligament
C) broad ligament (hangs down either side = fold of peritoneum)
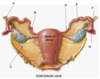
Label the 2 peritoneal pouches

A) vesicouterine pouch
B) rectouterine pouch (Douglas pouch), can accumulate pus/blood, can be drained through anterior wall of vagina
What is the broad ligament?
Where are the ovaries attached? Where do they lie?
Where is the suspensory ligament?
Wide fold of peritoneum that connects the sides of the uterus to the walls and floor of the pelvis.
The back of the broad ligament by the mesovarium. Lie in the ovarian fossa (varies greatly - could be in Douglas pouch)
The part of the broard ligament extending between the mesovarium and the lateral wall of the pelvis.
Label A-G in this posterior view of the uterus.
A) suspensory ligament (vessels)
B) ovarian/round ligament
C) broad ligament (mesometrium)
D) isthmus
E) ampulla
F) infundibulum
G) fimbriae
What are the supports of the uterus?
Levator ani muscles and perineal body
Transverse cervical (cardinal) ligaments (largest)
Pubocervical ligaments (from front)
Sacrocervical ligaments (from back)
Damage to these = main cause of uterine prolapse
Describe the vagina.
What relations and supports are found anterior, posterior and lateral to the vagina?
What are ureters?
Thin muscular tube extending backwards from vulva to uterus, upper half above pelvic floor, lower perineum. Upper end of vagina pierced by cervix divided into fornices - ant, post and 2 lateral.
Anterior: bladder/urethra. Posterior: pouch of Douglas, ampulla of rectum, perineal body. Lateral: ureters, levator ani, urogenital diaphragm, bulb of vestible
Retroperitoneal muscular tubes, pass over pelvic brim at bifurcation of common iliac arteries in front of sacroiliac joint, oblique entrance into bladder - one way flap valve.
Label A-G

A) fallopian tube
B) suspensory ligament - contains ovarian vessels
C) ureter
D) ovary
E) cervix
F) bladder
G) round ligament


