Neuropathology 1 Flashcards
(192 cards)
1) The Fasciculus Gracilis exist at _______of spinal cord and DOES contain ______ ____ from the ___
vs.
Fasciculus Cuneatus exist in {__-__} = ____ and ______ and contains _____ ____ from the ___
1B) Which Pathway are these Fasciculus columns associated with?
2) What happens to 2nd order neurons of this Pathway?
2B) Where are these 2nd order neurons located?
3) What happens to 3rd Order neurons of this Pathway?
4) How does [Proprioreception/Vibration/2-point discrimination] get to 2nd order neurons? [5]
**Position/Vibration/2-point discrimination travels from periphery in the ______ ______—–> passes ______—>passes ______ ______ Gray mater–>ultimately travels upwards using ______ ______ or ______ ______
—>travel up into [______ MEDULLA] to synapse 1st time in ______ ______ or ______ ______
1) The Fasciculus Gracilis exist at ALL LEVELS of spinal cord and DOES contain [ascending sensory fibers] from the LE
vs.
Fasciculus Cuneatus only exist in {C1-T6} = Thoracic segments (T1-T6) and Cervical segments (C1-C8) and contains [ascending sensory fibers] from UE
**DORSAL COLUMN PATHWAY**
2) 2nd order neurons in [nucleus gracilis] AND [nucleus cuneatus] decussate as [internal arcuate fibers] in LOWER MEDULLA—>cross midline to form [Medial Lemniscus]—>this travels to VPL nucleus of thalamus!
3) 3rd order neurons in [VPL nucleus of thalamus] travel in internal capsule and terminate in [Area 312 POSTcentral gyrus]
4) Position/Vibration/2-point discrimination travels from periphery in [Dorsal Root]—> passes DRG—>passes Dorsal Horn Gray mater–>bends in {Fasciculus cuneatus or gracilis}—>travel up into [LOWER MEDULLA] to synapse 1st time in {nucleus cuneatus or gracilis}
A) [Lateral Dorsal Root] Synapses in ____ _____ of ____ Horn and then becomes the _____ ______ . What sensations is this transmitting? [2]
B) SPINOTHALAMIC TRACT DECUSATES in _____ _______ and BEGINS ASCENT in the __________
—->It then travels ultimately travel up to [VPL nucleus of Thalamus] via the _____ _____ of spinal cord
C) Cutting STT in CORD will affect Pain on ____[same/Opposite] side of Body
A) [Lateral Dorsal Root] Synapses in Nucleus Proprius of [Gray Dorsal Lateral Horn] to become SPINOTHALAMIC TRACT= USED FOR PAIN and TEMPERATURE OF THE BODY
B) SPINOTHALAMIC TRACT DECUSATES in [ANT Commissure of Spinal Cord] and begins ascent in the [white Anterolateral Fasciculi] —->STT then ultimately travels up to [VPL nucleus of Thalamus] via [LATERAL FUNICULUS] of spinal cord
C) Cutting STT in CORD will affect Pain on OPPOSITE of Body

A: [Dorsal Spinocerebellar tracts] travel in ____ ______ and synapse either on _____(below C8) OR _____(Above C8). This tract is used for ____ ______ ______
B: Muscle Spindles use Sensory Affarent fibers (which bend in the [Fasciculus ______]) and transmit __ ______ ______ to the [____ _____ _____ nucleus] located in ___ ______
C: What is the [cuneocerebellar tract] ?
**A tract that receives ______ info from ______ nucleus & then ______[contralaterally/Ipsilaterally] sends this to the __ ___ ____ which relays info to ______ ______
D: [Dorsal Spinocerebellar tracts] AND [cuneocerebellar tract] use the__ ___ ____ to enter Cerebellum Vermis
A: [Dorsal Spinocerebellar tracts] travel in LATERAL FUNICULUS and synapse either on [Dorsalis Nucleus of Clarke] (below C8) OR lateral accessory cuneate nucleus for UNCONSCIOUS IPSILATERAL PROPRIORECEPTION
B: Muscle Spindles use Sensory Affarent fibers to bend in the [Fasciculus CUNEATUS] and transmit UE unconscious positioning to the LACN [lateral accessory cuneate nucleus] located in Lower Medulla.

C: [cuneocerebellar tract] = tract that receives UNCONSCIOUS positioning info from LACN [lateral accessory cuneate nucleus] & then ipsilaterally sends this to the ICP—> Cerebellum VERMIS
D: [Dorsal Spinocerebellar tracts] use the [inferior cerebellar Peduncle] to enter Cerebellum Vermis
A: How are the Bipolar Cells, Internueonrs & Ganglion cell bodies arranged near the Fovea? What about blood vessels?
B: How does Fovea and surrounding Macula receive metabolic supply?
C: Fovea is an _____[vascular/Avascular] retinal area with the ___[least/most] visual acuity. It has a __ ___ ____layer to prevent light barrier and is EXCLUSIVELY _____. There is a 1:1 ratio with [__:___] -which means ___ are more specific
D: Fovea is only __% of Retina and transmits __[least/most] of visual information to ________
A: Near Fovea, Bipolar Cells, Interneurons & Ganglion cell bodies are pushed LATERALLY–>makes a clear path for light = High visual acuity.
**Fovea is also Devoid of any blood vessels for same reason
B: Since Fovea is Devoid of any blood vessels, Fovea and surrounding Macula depend on diffusion from underlying choroid vessels for metabolic needs
C: The Fovea is an AVASCULAR retinal area with the MOST visual acuity. It has a laterally flat inner layer to prevent light barriers and is EXCLUSIVELY CONES. There is a 1:1 ratio with
[ganglion cell body: Cone receptor] –>Cones are more specific!
D: Fovea is only 5% of Retina but transmits MOST of visual information to [Lateral geniculate nucleus of thalamus]

A: What are the 7 Steps of Visual Pathway starting with light entering eye?
B: Light Entering Eye:
[TEMPORAL Field axons] pass _____ [crossed/uncrossed]
vs.
[nasal field axons] pass ____ [crossed/uncrossed], which means what for optic chiasm lesions?
A: Pathway of Visual Info from Retina [RN CT L DV]
“RN (use) CT (to) Learn Direct Vision”
1st: Light enters —> hits Retina
2nd: Travels in Optic N.
3rd: Optic Chiasm [Temporal Field Axons CROSS HERE]
4th: Optic Tract
5th: [Lateral Geniculate Nucleus of Thalamus]
6th: Optic RaDiations [Meyer’s Temporal Loop vs. Parietal direct path]
7th: [Area 17 -Calcarine Primary Visual cortex]
B: Light Entering Eye:
TEMPORAL Retina Fields pass CROSSED = [Temporal fields] decussaTe at Optic Chiasm
vs.
nasal retina fields pass UnCrossed @ Optic Chiasm = NOT AFFECTED BY Central OPTIC CHIASM LESIONS

A: [P-type] ganglion cell bodies are used by _____. [M-type ganglion cell bodies are used by ______.
B: Describe each of these
[2 each]
A: There are 2 MAJOR classes of [innermost ganglion cell bodies]
1. P-Type [USED BY CONES] “Pretty Colors”
ºsmall receptive fields –> BEST with [color/fine detail/high acuity]
ºtons of it near Fovea
- M-type[used by rods]
ºLARGE Bodies and many axons share 1 cell body –> LARGE Receptive fields
ºBEST with [rapidly transient adaptation] &response to mvmnt or large objects
A: Although Visual Perception begins in ______, collateral visual info enters ____ via Pretectal Area= for ___ _____ and _____ _____ for ________
B: Pretectal Area uses ___ nuclei of _____ for ___ _____ and projects both ipsilateral & contralateral via ____ _____
A: Although Perception of vision begins in [Area 17 CPVC-Calcarine Primary Visual Cortex] collateral visual info enters
- Brainstem via Pretectal Area=FOR PUPILLARY REFLEX and
- [SUP Colliculus]=For [head&eye movement]
B: Pretectal Area uses [Edinger-Westphal nuclei] of midbrain for PUPILLARY REFLEX and projects both ipsilateral & contralateral via POSTERIOR commissure
What would occur if there was a Lesion in …
1. R Optic N. —->
- *Optic Chiasm —–>
- R Optic Tract—>
- R [lower radiation meyer’s loop] –>
- R [Lateral Geniculate nucleus of thalamus]–>
- R [upper radiation fibers]
- R [Area 17 CPVC]
B: Which 2 lesions present the same Visual sx?
C: Which Visual Field Decussates at Optic Chiasm?
Lesion in … (using R side damage as example)
- R Optic N. —-> BLIND RIGHT EYE
- ——————————————————————————- - *Optic Chiasm —–> [Bitemproal Heteronymous hemianopsia] (both temporal fields knocked out) since Temporal fields decussaTe at Optic Chiasm
- ——————————————————————————- - R Optic Tract—>[CTL homonymous hemianopsia]
- ——————————————————————————- - R [lower radiation meyer’s loop] –> “Pie in the Sky Lesion’ = [CTL homonymous upper quadrantanopsia]
- ——————————————————————————- - R [Lateral Geniculate nucleus of thalamus]–>[CTL homonymous hemianopsia]
- ——————————————————————————- - R [upper radiation fibers]–>[CTL homonymous LOWER quadrantanopsia]
- ——————————————————————————- - R [Area 17 CPVC]–> [CTL homonymous hemianopsia with macular/fovea sparing]
- ——————————————————————————-

**Lesions of Optic Tract {4} and [Lateral Geniculate Nucleus of thalamus] {6} - PRESENT SAME VISUAL SX!
C: [Temporal fields] decussaTe at Optic Chiasm
CTL = Contralateral or (Left side in this case)
A: The Pupillary Light Reflex involves a ___ reflex and ____ reflex. Describe each?
B: After light is shone thru 1 eye, BOTH pupils constrict becuz ___ connections to [_____ nucleus] from ____ fibers traveling thru [___ ____]–> activates [Oculomotor CN3] fibers to synapse in the ___ganglion and constrict ____ _____ m.
C: What part of the brain does this test?
D: [Optic Nerve damage] presents how? Why is this?
vs.
E: [Oculomotor Nerve damage] presents how? Why is this?
A: DIRECT reflex = light is shone thru L pupil and the L pupil constricts
CONSENSUAL reflex= light is shone thru L pupil BUT R pupil constricts also
B: both pupils constrict becuz bilateral connections to [Edinger-Westphal nucleus] from optic nerve fibers traveling thru [SUP colliculus] activates [Oculomotor CN3] which travels to Ciliary ganglion ipsilaterally—>constrict [sphincter pupillae m].
C: Rostral Midbrain
D: Optic Nerve Damage—-> EQUAL PUPILS becuz signal is NEVER sent to [Edinger-Westphal nucleus]= NO REFLEX on either side
vs.
E: [Oculomotor CN3] damage—>[constricted pupil on 1 side and Dilated pupil on other]. Signal is sent from Optic N. but only 1 [Oculomotor CN3] is working = 1 sided constriction

A: Explain how the [Pupillary Dark Reflex] is transmitted?
B: Explain what causes Horner’s Syndrome and the 4 manifestations?
A: Darkness activates [Optic Tract] which –> terminates at hypOthalamus –> hypOthalamus sends its axons to descend in spinal cord and terminate at the [sympathetic preganglionic neurons of the T1-T3 lateral horn]–>sends its axons to [SUP cervical ganglion]–> Postganglionic axons in the [ciliary n.] –> Activate [iris Dilator pupillae m.]
B: Horner’s Syndrome= Damaged [SUP cervical ganglion]
1) loss of [Face Vasculature] –> flushing
2) loss of [Sweat/Lacrimal glands] –> (anhidrosis)
3) loss of [Eyelid Tarsal Muscles]—> (Ptosis)
4) loss of [iris Dilator pupillae m.] –> (miosis)

In order to change gaze & focus on very close objects you need the ____ REFLEX, which involves what 3 things?
In order to change gaze & focus on very close object you need the ACCOMMODATION REFLEX which involves..
1. eye convergence via [medial recti m.]
- Ciliary m. constriction —>Lens thicken
- Constriction of both pupils–>DEC light entering due to greater reflectance from close object

A: What are the 2 ways to Detect Motion?
B: *Motion Perpendicular to orientation axis can be detected by____ ___ ____ but___ ____is needed for more complex movements **
C: What test is used to test for Color Blindness?
2 ways to detect Motion
1. Image moves temporarily across retina while eye remains still = “temporal association”
- [Head & Eyes] move to fix the [object image] onto the fovea
B: *Motion Perpendicular to orientation axis can be detected by [Area 17 CPVC] but [V5 Temporal area] is needed for complex movements **
C: Ishihara Test
**DIFFERENCES BETWEEN RODS & CONES **
1. ____ are better for DAY Vision with ___[higher/lower] sensitivity to light. They Saturate only in _____ Light
- ____ Capture MORE light and are great for _____ Vision and ______ light. ___ have ___[FAST/slow] response time and long integration.
- Cones have Less photopigment AND Less amplification per cell
- ___ are AChromatic and ____ are Chromatic ! Explain this
- Which photoreceptor CAN’T do Bright Light?
- CONES are better for DAY Vision with Lower sensitivity to light. They Saturate only in INTENSE Light
- RODS Capture MORE light and are great for NIGHT Vision and Scattered light. Rods have slooow response time and long integration.
- Cones have Less photopigment AND Less amplification per cell
- Rods are AChromatic and Cones are Chromatic!
**Chromatic Cones = 3 types of photopigment in Cones (each sensitive to diff visible light spectrums –> Red/Blue/Green
**AChromatic Rods= ONLY 1 TYPE of photopigment in Rods
- RODS CAN’T DO BRIGHT LIGHT (since they capture more light)
A: In the OUTER ear the ___ & ______ direct sound/vibrations to tympanic membrane
B: Once in The MIDDLE ear _______ conduct sound from the tympanic membrane to the ___ _____
C: What does the EUSTACHIAN Tube do and where is it located?
A: In the OUTER ear the Pinna & [EAM Ear Canal] direct sound to the tympanic membrane
B: The MIDDLE ear [MIS ossicle bones]–>{Malleus/Incus/Stapes} conduct sound from tympanic membrane to the [Oval vestibular window]

EAM = External Auditory Meatus
A: [Bony Labyrinth] is the __-SHAPED CAVE of the ____ ear that surrounds a bony core called the _______. It’s housed in the ____ _______ bone and has a [_____ Snail Apex]. The [Bony Labyrinth] is divided into 3 canals.
B: These 3 Canals are separated by the ____ ___ _____ & ____ ___.
C: Describe These 3 Canals
A: [Bony Labyrinth] is the SNAIL-SHAPED CAVE of the INNER ear that surrounds a bony core called the [MODIOLUS]. It’s housed in the Petrous temporal bone and has a [Helicotrema Snail Apex]. [Bony Labyrinth] is divided into 3 canals.
B: 3 Canals: [Scala are separated by [Reissner’s Vestibular Membrane] & basilar membrane]
1. Scala Vestibuli (Contains perilymph & is continuous with bony labyrinth of vestibular apparatus)
- Membranous Labyrinth (contains _endo_lymph and is inbetween 2 Scala)
- Scala Tympani (Contains perilymph and separated from Cochlear Duct by Basilar membrane of the round window)

A: [Membranous Labyrinth] is filled with ______ & forms the ___ ____ (or ___ ____) which contains [________]. This is where __________
B: How far does the Cochlear Duct extend throughout the cochlea in the [Membranous Labyrinth]?
A: [Membranous Labyrinth] is filled with ENDOLYMPH & forms the COCHLEAR DUCT (or scala media) which contains [Organ of Corti]. This is where sound wave transduction—>nerve impulses occur.
B: Cochlear Duct extends throughout the cochlea, EXCEPT FOR HELICOTREMA

1) The [Organ of Corti] contains __inner row and __ OUTER rose of hair cells. Describe each of these rows (OUTER vs. inner row)
2) What are Stereocilia
3) Is hearing an Active or passive process?
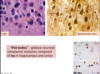
[Organ of Corti] contains 1 inner row and [3 OUTER ROWS] of [hair cell cilia]
*OUTER ROW= contain Stereocilia that insert into tectorial membrane & can receive inhibitory inputs via olivocochlear n. fibers= amplifies/sharpens/suppresses responsiveness of inner row
*inner row= When cochlear fluid displaces Basilar membrane–>displaces Tectorial membrane—-> deflects [Stereocilia of inner row to move in endolymph]–> TRANSDUCTS MOST OF SENSORY AFFERENT VIA CN8
2) Stereocilia= [Tethered Hair cell cilia] arranged in a “V” and when 1 is bent –> causes neighboring Stereocilia to bend
3) Hearing is an ACTIVE PROCESS

•Cochlear nerve fibers enter brainstem at ___ _____ and terminate in ___________
B: Ventral cochlear nucleus is ___[smaller/Larger] and it projects to to the _______ nuclei in the _____. What is the TRAPEZOID BODY?
C: dorsal cochlear nucleus terminates in the ___ and ____ nuclei
D: [inferior Colliculus] relays ____ info (via ____) to_____ nucleus in the Thalamus —->sends ______ projections to _______ where it is interpreted
E: [T or F] Auditory Cortex is sensitive to lesions and can easily —> sound discrimination problems
•Cochlear nerve fibers enter brainstem at PONTOMEDULLARY JUNCTION and terminate in [Dorsal/Ventral cochlear nuclei]
B: Ventral cochlear nucleus is LARGER and it projects to ipsilateral & contralateral [SUP olivary nuclei] in Pons. **Midline crossing of the [Ventral cochlear nuclei] axons = TRAPEZOID BODY
C: dorsal cochlear nucleus terminates in the [inferior Colliculus] and [lateral lemniscus nuclei]
D: [inferior Colliculus] relays auditory info (via brachium) to [Medial Geniculate nucleus] in Thalamus —->sends auditory projections to [Area 41 Heschl’s Gyri]
E: FALSE! Auditory Cortex Lesions have to be EXTENSIVE in order to affect sound discrimination

C: Where is the Tensor Tympani m. & what is it innervated by?
D: Where is the Stapedius m. & what is it innervated by?
D2: What is the OVERALL PURPOSE of these 2 Middle ear muscles?
C: Tensor Tympani m.= Fast Striated m. (middle ear wall fibers) near eustachian tube that attaches to Malleus
{{Innervated by CN5B3}}
D: Stapedius m.= Fast Striated m. (middle ear wall fibers) tht attaches to [Stapes] near its connection with [Incus]
{{{Innervated by Facial CN7}}}
D2: Purpose of these MIDDLE EAR m. is to DEC amplification of sound oscillation—> protect us from LOUD SOUNDS & adjust loudness of voice b4 we speak[using Facial CN7]

A: Describe the Semicircular Canals
C: Utricle and Saccule are Dilations of the __ ___ that contain _____ which allows them to ______ . Why can they do this? How are they related to the Maculae?
D: What’s the difference between Utricle and Saccule in regards to Planes?
E: ºThe ______ [Utricle/Saccule] connects the [3 semicircular canals]
ºThe ______[Utricle/Saccule] is continuous with Cochlea
ºBOTH Utricle & Saccule have an ______ ______ for [______, ______ & ______ detection]
A: 3 interconnected tubes positioned at right angles to one another in 3 planes of space (1 horizontal, 2 perpendicular)

C: Utricle and Saccule are Dilations of the [Membranous Labyrinth] that contain [Ca+carbonate Otolithic granules]—>allows them to respond to gravity/acceleration because it Adds weight. They also EACH have a Maculae which contains the [Vestibular sensory Hair cells]
——————————————————————————
1. Utricle = sensory hair cells oriented in HORIZONTAL plane = sensitive to linear acceleration/deceleration in HORIZONTAL DIRECTION
-
SACcule =sensory hair cells oriented in vertical plane = sensitive to linear/acceleration/deceleration in VERTICAL DIRECTION. “We SAC those dudes Vertically”
- ——————————————————————————
E:
ºThe Utricle connects the [3 semicircular canals]
ºThe Saccule is continuous with Cochlea
ºBOTH have an Otolithic Membrane for [Gravity, Acceleration & position detection]
[PPRF] Paramedian pontine reticular formation
1. Where is this located?
- What happens when this is stimulated?
- Describe its projection
- ——————————————————————————- - Explain what the [mesencephalic reticular formation] does and is located?
- A: Vestibuloocular Reflexes (VORs) reflexly move eyes in Direction ____ of Head mvmnt. It uses ____ to get from ____ and ____ to the ____
B: Absent of (VORs) means there is ___ damage
[PPRF] Paramedian pontine reticular formation
1. Near abducens nucleus (so sometimes called parabducens nucleus)
- Stimulation = Horizontal Eye movement
- Receives multiple afferents and projects to Ocular nuclei 3, 4 and 6 using the [Ascending MLF]
- ——————————————————————————- - [mesencephalic reticular formation] = includes a [Cajal interstitial nucleus] and controls VERTICAL eye mvmnt . Is located in the ROSTRAL [PPRF]
- A: Vestibuloocular Reflexes (VORs) reflexly move eyes in Direction OPPOSITE of Head mvmnt. It uses [Ascending MLF] to get from [medial vestibular nuclei] and [SUP vestibular nuclei] —->PPRF—>[CN nuclei 3, 4 & 6]
B: Absent of (VORs) = brain STEM damage

What are the 3 ways we can get “Dizzy”?
- Vestibular input without vision (i.e. spinning in a chair with eyes closed–> constant motion that eventually results in cupola membrane returning to its baseline)
- [Motion detection from Visual system] but WITHOUT [Vestibular confirmation] (looking out car window when an adjacent car moves away= false sense of motion)
- [Motion detection from Vestibular system] but WITHOUT [Visual confirmation] (sitting in cabin of a boat during a storm= MOTION SICKNESS)
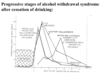
Nystagmus are __ ___ ___ that have both _ and __ components (but during test refers to ___ component only) *There are 3 types*
B1. SPONTANEOUS Nystagmus is ____[sometimes/always] pathological and is caused by ___ ____ 2º to ______
B2. What are the 3 sx?
Nystagmus are OSCILLATING EYE MOVEMENTS that have both slow and Fast components (but test refers to Fast component only) .
B1. SPONTANEOUS Nystagmus is ALWAYS PATHOLOGICAL and is caused by [Vestibular/ Brainstem/ Cerebellum] imbalance 2º to irritating or destructive lesions.
B2: Sx= [N/V] + [bp DEC] + Tachycardia
A: Tracking/Smooth Pursuit involves _____ using ______. Is Tracking/Smooth Pursuit voluntary and can it be done without Visual Stimuli?
B: What is the [Fixation Reflex]? Give example
C: [Optokinetic Railway Nystagmus]? Give example
A: Tracking/Smooth Pursuit involves “Locking” eyes onto perceived moving object using [Occipital Eye Fields]. Although These mvmnts are voluntary, smooth sweep of eyes CAN’T be done in ABSENCE of visual stimuli
B: Fixation Reflex = same as smooth pursuit mvmnt but allows us to fix on an object when BOTH person AND object are moving [Ex: Reading road sign while driving on bumpy road]
C: [Optokinetic Railway Nystagmus] = (to-and-from) oscillating eye mvmnts made when ur fixating on moving objects [Ex: Looking @ telephone pole out window of moving train]